HIIT Training – Physiology
Home » Fitness Training »

By Dan Speirs
This HIIT Training Physiology article is part of our ‘Technically Speaking’ series which is a deeper look at a particular topic. A video lecture is available.
We’ve covered the benefits of High Intensity Interval Training and HIIT protocols already.
HIIT training benefits
- more effective at developing aerobic fitness than medium intensity continuous training
- reduces body fat, including reducing visceral fat (fat around the organs and waist)
- is most effective for people with low to average fitness, and as effective as other forms of training for the very fit
- significantly improves insulin sensitivity (circa 20-60%)
Anatomy of a HIIT workout
HIIT Physiology
In this article we are going to explore the exercise physiology behind HIIT to discover why the training has the myriad of effects it does.
Prefer to watch a video?
Now we know what a HIIT workout might look like on paper, we need to understand what happens when we train this way.
We need to know:
- How does the body respond to the work period
- What is happening during the relief period
- What effect the duration and intensity of each the period (work and relief) has on the training response
Understanding the HIIT training response – the work period
First, let’s deal with the intensity of the work period.
Figure 7 is a graph of heart rate and intensity.
In this example the 30-year-old recreational runner has a maximal heart rate of 190 beats and attains VO2max when running at 16km/h.
You can see as the intensity increases (in this case running speed measured in km/h on the X axis), heart rate (on the y axis) increases in a linear fashion as the working muscles need more oxygen.
If we produce the graph again, we can add a second axis and line (red), which is the lactate curve.
Lactate accumulates rapidly as exercise becomes more intense.
You can see the lactate level in the runner’s blood begins to increase at a pace of 12 km/h (marked as OBLA – onset of blood lactate accumulation – sometimes noted as LT1).
Blood lactate starts to rapidly rise when the runner hits the 14 km/h pace (marked as LT and also called LT2 at times).
- OBLA (LT1) is the aerobic threshold
- Lactate Threshold (LT2) is the anaerobic threshold
HIIT uses each of these tipping points in cellular energy production.
Protocols are designed so lactate is produced and then either cleared/or accumulated over the workout.
What’s happening in the working cells during HIIT?
To understand how HIIT works we need to understand what’s happening in the muscle cell (and other cells around the body) during exercise.
We want to know what is;
- happening in the cell that causes OBLA (LT1)?
- occuring in the system at the Lactate Treshold (LT2)?
What is lactate and where does it come from?
Cells use fat and carbohydrates as their main energy sources.
Those macro-nutrients are broken down to smaller molecules which are then used to produce ATP (adenosine triphosphate). ATP is the energy currency of all living cells.
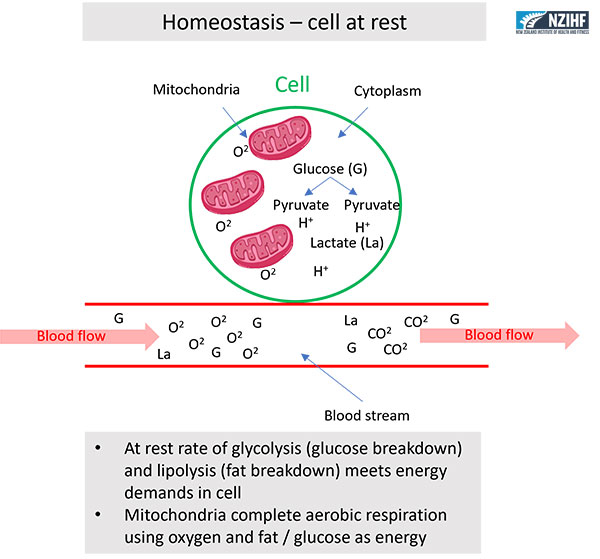
Sticking with glucose metabolism, we can produce ATP by breaking down glucose in the cytoplasm (see figure 11) producing net 2 ATP.
We can further take those breakdown products into the mitochondria (the cells major power plant) to produce more ATP (about 37 ATP).
What happens in the cell during rest – the physiology of the HIIT relief period?
Usually the rate of glycolysis (glucose breakdown) in a cell cytoplasm (the bit inside the cell wall) happens slowly enough that the majority of the cells energy can be produced aerobically (using oxygen).
That means, when glucose is split into pyruvate and hydrogen ions (H+), there is oxygen available to bind to the hydrogen (eventually forming H2O – water).
You can see this in figure 11 which represents energy production for a cell ‘at rest’ where there is ample oxygen and glycolysis isn’t happening that fast.
Here you can see glucose is broken down to pyruvate and H+ ions are produced.
There is ample oxygen available inside the cell and oxygen supply to the muscle cell is sufficient.
Because oxygen is present and glucose isn’t being broken down very fast, very little lactate is produced.
This means blood lactate in the surrounding tissues is stable.
What happens when we exercise hard – the physiology of the HIIT work period?
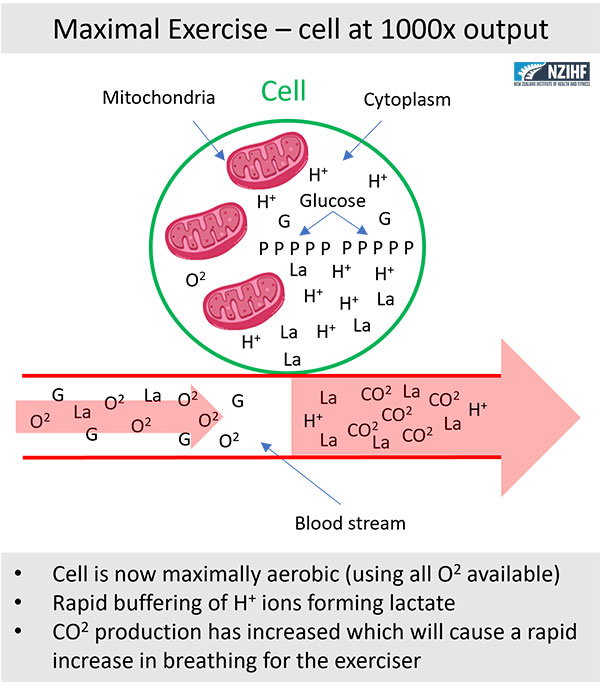
When a cell starts to work intensely to meet an exercise demand (such as the work period in a HIIT workout) the production of lactate changes as in Figure 12.
Here you can see the cell’s energy production is maximal (ATP production in cells can reach 1000x the resting production), with more lactate and H+ in the cell as glycolysis (the breaking of glucose to pyruvate) has accelerated dramatically.
In this cell:
- Lactate is leaving the cell and flowing into the blood.
- OBLA (LT1) has occurred as blood lactates are now higher than rest.
- Although the supply of oxygen has increased in the blood, the rate of glycolysis in the cell results in both maximal aerobic energy production and significant anaerobic energy production.
- CO2 (carbon dioxide) is increasing in the blood as well because the mitochondria are maximally recruited to produce ATP aerobically which produces significant CO2.
Okay, so we can see lactate is buffering hydrogen ions in the cell for a while, but as intensity increases or is maintained for some time, both lactate and H+ will eventually spill into the blood.
So we can say at a certain intensity we get OBLA which is what the graph in Figure 8 showed us about our runner.
Remember, the runner began to accumulate lactate (and H+) in the blood at a work rate of 12km/h.
What is the burning we feel when we sustain a hard bout of exercise during HIIT training?
Because lactate is a buffer of H+ ions (hydrogen ions), and H+ ions are acidic as they lower the pH in the system (a lower pH – potential hydrogen – is a measure of acidity), we eventually feel burning when the lactate can’t buffer all of the H+ ions produced by glycolysis. Note, there are other H+ buffers but lactate is does the majority of the work.
Lactate is actually a neutral substance. Lactate is not an ‘acid’. It just so happens that we measure and talk about lactate because we know as the buffering capacity of lactate is overwhelmed, the acidity in the tissues increases. The burning isn’t the lactate, it’s the unbound H+ ions.
Blaming lactate for the burn is like blaming the fire department for the fire. They turned up to put it out, but they didn’t start it.
What happens if we keep exercising while lactate accumulates?
So far, we’ve discovered why OBLA (LT1) occurs and that it represents the ceiling of our ability to produce energy aerobically in the working cells. Hence, it’s called the aerobic threshold.
But, what about the Anaerobic Threshold (confusingly also called Lactate Threshold and more correctly LT2)?
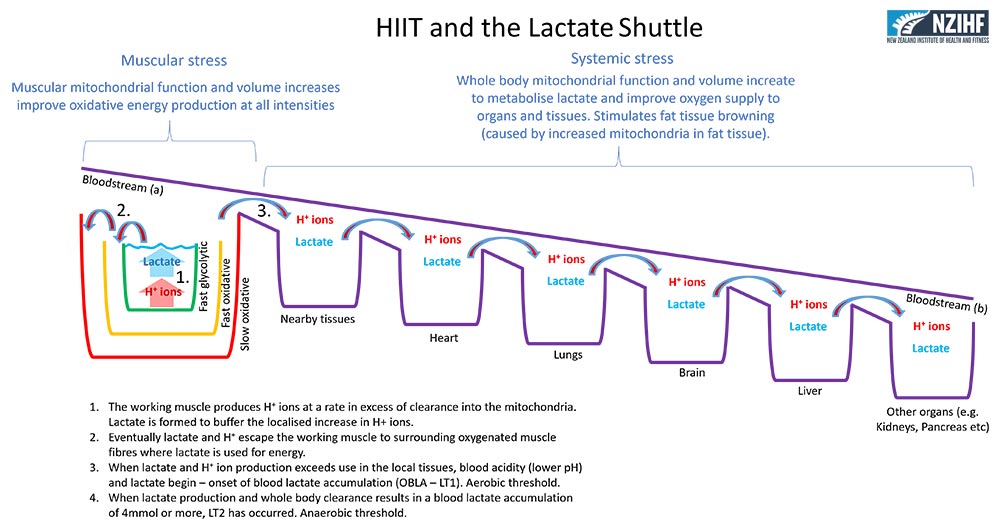
To understand LT2 we need to understand the bodies ‘Lactate Shuttle’ as depicted in Figure 10.
I like to think of the lactate shuttle as the body’s way of distributing potential energy.
When pyruvate buffers H+ it becomes lactate and you end up with a neutral molecule that can be transported in the blood to any oxygenated tissue for use.
Lactate is still a fuel, it just needs oxygen to peel off the H+ ion and it’s back to the highly desirable pyruvate.
What the lactate shuttle shows us is that the working muscles rapidly produce H+ ions and lactate.
Then that lactate then flows into surrounding oxidative muscle fibres to be used.
If the lactate continues to accumulate, it can spill from the local tissues into the bloodstream where nearby tissues and organs can use that lactate as a fuel.
It is only when lactate elimination (use by all oxygenated tissues) cannot keep up with lactate production that lactate accumulation occurs.
So, lactate is a buffer (locally) and a fuel (globally).
This is a very biologically efficient set up.
The output of rapid energy use in the working cells becomes a supply chain for almost immediate energy, in the form of lactate, in other oxygenated tissues.
What is Lactate Threshold (LT2)?
We’ve established that LT1 (OBLA) is the point at which lactate starts to accumulate beyond resting levels in the blood.
Now with our understanding of the lactate shuttle we can see that LT2 occurs when whole body lactate clearance, by all oxygenated tissues and organs, cannot reduce the blood lactate.
Effectively, as the working tissue produces more lactate, the blood lactate climbs in a linear fashion.
Generally, 4mmol/L of blood lactate is accepted as the ‘tipping point’ where gradual increases in blood lactate transition to rapid increases in blood lactate that relate directly to increased muscular work.
Think of it this way.
Current circulating lactate – cleared lactate + new lactate produced = net lactate at working tissue (mmol/L)
Current La – Cleared La + New La = La at tissue
- Exercising sub-maximally; 2 (new La) + 1 (existing La) – 2 (cleared La) = 1 mmol/L no change in blood lactate
- Exercising at / just above OBLA (LT1); 3 (new) + 1 (existing) – 2 (cleared) = 2 mmol/L OBLA has occurred
- Exercising at / above LT2; 5 (new) + 1 (existing) – 2 (cleared) = 4 mmol/L LT2 is occurring
At LT2 the cell and circulation might look like Figure 13.

Figure 13: Cell at sustained maximal effort with rapid accumulation of lactate in system. Click to enlarge.
Summary of acute physiological responses to HIIT
You can see the acute response to HIIT is:
- Increased oxygen intake and supply to the muscle for use in the mitochondria and across all tissues
- Breathing rate and depth increases (due to the CO2 coming from working cells, into the blood)
- More lactate production in the cells due to fast glycolysis
- Increased buffering of H+ ions by the formation of lactate within the cell
- More lactate in the blood if production is greater than whole body clearance
- Glucose uptake into working cells increases
- Up regulation of the use of lactate as a fuel in oxygenated tissues
- Increased heart rate, stroke volume, vasodilation (opening of blood vessels) to get blood to and from the working tissues
- Maximal use of the cells mitochondria for oxidative phosphorylation (burning of fat and carbohydrate)
This myriad of responses occur in response to the intensity of the work and the H+ ions present.
The key here isn’t necessarily massive systemic accumulation of lactate. That is traditionally how HIIT has been approached.
The key is to maximally stress the working cell to produce lactate, that leaves the cell and is cleared by other oxygenated tissues.
In this way, you are achieving local adaptations in the working tissue (the cells doing the work producing the forces needed for exercise). And, you are achieving aerobic adaptations in central tissues including circulation and other organs (such as brain, kidneys, heart, lungs, liver and so on).
Understanding this is critical to a more progressive understanding of HIIT. You can use LT2 and accumulate massive lactates if you want to. However, you don’t need to do that to get the benefits of HIIT. You can train around OBLA using very high intensity bursts of activity and longer rest periods which is more comfortable and still very effective. We cover this in more detail in the HIIT design articles.
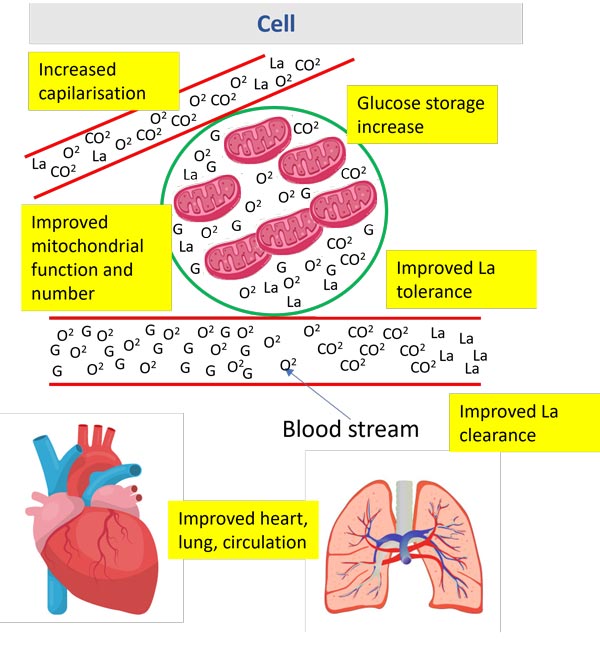
Chronic physical adaptations to HIIT
With all exercise, if you repeat the stimulus regularly over time, your body will adapt to that exact stimulus.
This is called the specificity principle in exercise. The acronym often used is SAID – specific adaptation to imposed demand.
Now that we understand the acute physiological responses to HIIT (the imposed demand) we can look at the changes (specific adaptations) that we can expect.
Because there are a lot of adaptations caused by HIIT I’ve split them into lumps that relate to their functions.
I haven’t covered all of the adaptations, but you should get the picture looking at figure 19 and the list below.
More oxygen
- More oxygen present in the cell – the tissues are more oxygenated at rest
- Greater oxygen content in the blood – the oxygen carrying capacity of the blood increases
- Oxygen passes into the mitochondria more readily – the transport of oxygen into mitochondria improves
More oxidative energy production
- More mitochondria – mitochondrial biogenesis increases the number and/or size of mitochondira
- Improved alignment of mitochondria – the mitochondria bind together to form a chain gaining efficiency
- Better functioning mitochondria – the mitochondria’s properties are improved during remodelling
More blood
- More blood gets to the cell as the capillaries become better at dilating (widening)
- Additional capillaries are laid down to the cell
- An increase in overall blood volume and haemoglobin content (the molecule that carries oxygen in the blood)
- Better pumping of blood by the heart with a larger stroke volume (the amount of blood ejected from the heart on a beat) and stronger heart muscle
- More lung capacity as the lungs expand and relax more readily, and stronger respiratory muscles in the rib cage to deal with rapid and deep breathing
Increased buffering and transport
- More CO2 out of the cell as the diffusion gradient (difference between blood and cell concentrations) improves
- Increased lactate transporter (l-lacate) to clear lactate from the cell
- Additional buffers for H+ ions as lactate isn’t the only hydrogen buffer
Improved storage
- More calcium storage in the mitochondria (calcium is used to stimulate muscle contractions)
- Increased glucose storage capacity in the cell
- Improved insulin sensitivity (more receptors and better function) so more glucose can get into the cell quickly
As a result of these adaptations cells become;
- More oxygenated
- Better at burning fat and lactate (both are released by fat stores)
- Adapted to produce more energy aerobically at any intensity (therein burn more fat at rest or during exercise)
- More capable of producing energy leading to a higher metabolism
- Efficient at metablolising glucose rapidly for energy increasing peak power and lactate capacity
Given the above adaptations it’s easy to see why HIIT has a dramatic effect on fat stores, retention of muscle, and whole-body health.
Physiology of HIIT Summary
- Working cells produce energy rapidly by splitting glucose into pyruvate
- Pyruvate can bind to excess H+ ions forming lactate
- Lactate can be transported to surrounding tissues and organs via the blood
- Other oxygenated tissues can use lactate as energy and reduce total blood lactate
- The rate of production and elimination of lactate dictates the blood lactate level at any time
- Blood lactate is indicative of H+ ion content of the blood and when this is high, the blood becomes acidic
- The acidity inhibits glycolysis and reduces energy production in the cell – this is a negative feedback loop
- Repeated bouts of HIIT cause cellular and systemic adaptations that optimise lactate and fat use at all intensities
- HIIT conditions the cells to be able to produce a lot of energy quickly and form a lot of lactate quickly both anaerobic adaptations
- Because the work period is intense lean tissue mass (muscle) is often preserved
More information on HIIT training
Search our website for more articles and videos on HIIT training and more.
Subscribe to get great content direct to your inbox.
Here’s a glossary of technical terms used in this HIIT training article
1. Maximal aerobic power – the maximum amount of oxygen the body can use to produce energy in the cells
2. Aerobic – is the energy produced by the cell with the use of oxygen
3. Anaerobic – is the energy produced by the cell without the use of oxygen
4. HIIT – high intensity interval training
5. SIT – sprint interval training
6. RST – repeated sprint training
7. VO2max – maximum volume of oxygen the body can consume per minute stated as ml/kg/min (millitres per kg of body weight per minute)
8. OBLA (LT1) – onset of blood lactate being the point at which blood lactate deviates from resting values
9. Lactate threshold (LT2) – the point at which blood lactate rapidly accumulates in a linear fashion when related to work intensity
10. Aerobic threshold – the point at which the working tissues are generating energy beyond their aerobic capacity and usually measured as the OBLA/LT1
11. Anaerobic threshold – the point at which anaerobic energy production in the muscle far outweighs whole body clearance of lactate resulting in rapid increases in blood lactate usually indicated as LT/LT2
12. Interval –where the person is active during the relief period of a repeat
13. Intermittent – where a person is entirely inactive during the relief period of a repeat
14. Mitochondria – the organelle in a cell that is responsible for producing energy (ATP) for cellular work aerobically
15. Oxygen deficit – a measure of the difference between the work produced and the aerobic energy produced indicating the amount of work done anaerobically
16. MAOD – is the maximum aerobic oxygen deficit is a measure of how much energy was produced anaerobically
17. Heart rate – the number of beats the heart makes usually stated as beats per minute (BPM)
18. HIIT Work Period = the time spent at work intensity
19. HIIT Relief Period = the time spent at relief intensity
20. HIIT Mode = is the type of exercise being done
21. HIIT Duration = the amount of time spent in a period
22. HIIT Intensity = how hard the exercise is in a period
23. Homeostasis = the stable (sometimes called resting) state of the body’s systems
24. ATP = adenosine triphosphate the energy currency of all cells
These are references used for this high intensity interval training (HIIT) article
[ref.1] Journal of Obesity Volume 2011, Article ID 868305, doi:10.1155/2011/868305
[ref.2] Tabata I, Nishimura K, Kouzaki M, Hirai Y, Ogita F, Miyachi M, Yamamoto K (1996) Efects of moderate intensity-endurance and high intensity-intermittent training on anaerobic capacity and VO2max. Med Sci Sports Exercise 28:1327–1330
[ref.3] E. G. Trapp, D. J. Chisholm, J. Freund, and S. H. Boutcher, “The effects of high-intensity intermittent exercise training on fat loss and fasting insulin levels of young women,” International Journal of Obesity, vol. 32, no. 4, pp. 684—691, 2008
[ref.4] Tschakert, G., & Hofmann, P. (2013). High-intensity intermittent exercise: methodological and physiological aspects. International journal of sports physiology and performance, 8(6), 600-610.
[ref.5] D. Wen, T. Utesch, J. Wu, et al.. Effects of different protocols of high intensity inter-val training for VO2 max improvements in adults: A meta-analysis of randomised controlled trials. J Sci Med Sport (2019), https://doi.org/10.1016/j.jsams.2019.01.013
Use Your Passion for Fitness to Change Lives
Improve your own training, become a Qualified Personal Trainer and make a real difference in people's lives. Enquire now to find out more.













I loved the explanation, this video is so well done!